You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Historical Perspective
The concept of using computer-aided design (CAD) and computer-aided manufacturing (CAM) to restore teeth was introduced by François Duret, DDS, DSO, PhD, MS, MD-PhD.1 Another early pioneer, Werner H. Mörmann, BMD, DDS, PhD, successfully brought chairside CAD/CAM into the dental market with the CEREC® system (Dentsply Sirona, dentsplysirona.com). Later CAD/CAM systems were introduced by manufacturers including E4D (Planmeca E4D, E4D.com) and Carestream Dental (carestreamdental.com). In the early 1980s, resin composite materials lacked ability to resist wear and marginal degradation. Mörmann sought to predictably restore teeth with tooth-colored restorations that would be durable and esthetically pleasing.2 After the introduction of his first chairside CAD/CAM system in 1985 (CEREC 1), incremental improvements in software and hardware technologies over the subsequent 20 years established the concept of single-visit chairside CAD/CAM inlays, onlays, and crowns as predictable solutions for restoring damaged teeth.3 Yet after two decades of development and clinical documentation, CAD/CAM technology in dentistry remained a niche product for producing single-unit, same-day restorations.
CAD/CAM Technology Goes Mainstream
In the last 10 years, an enormous change has taken place in the scope of use for CAD/CAM and other digitally driven technologies in dentistry. Trends in use by dental laboratories have moved increasingly toward CAD/CAM workflows. Some of the most-used materials currently, such as zirconia and titanium, are being manufactured exclusively through CAD/CAM workflows. Today, even full-gold restorations and metal-ceramic frameworks can be manufactured more quickly and predictably with CAD/CAM, equaling or exceeding the fit of traditional cast restorations.4,5 Chairside CAD/CAM has evolved as well, now allowing the fabrication of fixed partial dentures, implant-related restorative solutions, and interaction with other digital technologies that facilitate the comprehensive treatment of patients in a digital space.
Developments in Digital Impressions and CAD/CAM Manufacturing
A persistent concern among dental professionals is the marginal fit of restorations; it is generally thought that poor marginal fit could contribute to sensitivity, recurrent caries, poor periodontal health, and restoration failure.6,7 Although there is no consensus on what should be considered a clinically acceptable marginal discrepancy, most literature examining the marginal fit for ceramic CAD/CAM restorations uses 120 μm or less or 100 μm or less as the benchmark for clinically acceptable.8 The fit of CAD/CAM restorations is primarily dictated by the quality of the digital data acquired during the digital impression, the size and geometry of the burs used to mill the subsequently proposed restoration, and the software that drives the process. Early CAD/CAM restorations, with a documented success rate of 90% at 10 years, often had a mean marginal gap of 200 μm or more.3 Although Fasbinder and others found significant marginal wear on occlusal surfaces of restorations, this wear was not found to contribute to restoration failure, recurrent caries, or sensitivity, and no significant marginal wear was found on axial or proximal surfaces.3 In fact, as early as a 2004 review, CAD/CAM-fabricated ceramics were found to have a lower annual failure rate than conventionally fabricated ceramics.9
The marginal fit of restorations produced with chairside CAD/CAM systems today is much better than with the early CAD/CAM restorations. Renne et al found the marginal fit and internal adaptation for restorations of both the CEREC and E4D CAD/CAM systems to be within the standard for clinically acceptable fit of less than 120 μm.10 As perhaps expected with any fabrication method, they found preparations with fewer preparation errors to have better-fitting restorations than those with more preparation errors.10 In another study, they found the marginal adaptation for IPS e.max® CAD restorations (Ivoclar Vivodent, ivoclarvivadent.us) fabricated with the E4D system (now the Planmeca Fit® system, planmeca.com) to be less than 40 μm given ideal crown preparations,11 similar to the marginal fit of pressed IPS e.max restorations documented in other studies.12,13 As pointed out in 2016 by Mounajjed and colleagues, heterogeneity in materials and methodology makes comparison difficult, but their review of in vitro studies of the marginal fit for IPS e.max restorations showed all restorations to exhibit a mean marginal gap that was clinically acceptable, irrespective of their fabrication method.8
Vast improvements have been made with the accuracy of intraoral scanners, which should further enhance the ability of CAD/CAM systems to produce quality outcomes. In a 2017 comparison of the trueness and precision of seven chairside scanners, some scanners were shown to be more accurate than some CEREC systems, which already have a proven track record of clinical success.14 Furthermore, Mennito and colleagues recently examined the influence of scanning patterns for sextant scanning, finding that most systems exhibited the same trueness and precision regardless of scanning pattern used.15 These findings reflect the accuracy and ease of use of digital scanners today. The findings have been confirmed by recent systematic reviews, which reported that restorations for fixed prosthodontics generated by digital impressions were equal to or better than those generated with conventional impressions with regard to preparation adaptation and marginal fit.16-18
Material Advances With Chairside CAD/CAM
The most commonly used materials in the early days of chairside CAD/CAM were either feldspathic ceramics, ie, the Vitablocs® Mark II by Vita (vita-zahnfabrik.com), or the leucite-reinforced ceramic IPS Empress® CAD from Ivoclar Vivadent. Lithium-disilicate ceramic IPS e.max CAD joined these other glass-ceramics in the late 2000s. The success of restoring teeth with bonded ceramics continues to be high, as reflected in a systematic review and meta-analysis from 2016, which found survival rates for ceramic inlays, onlays, and overlays high, regardless of clinical setting, length of study, or ceramic system used.19 Another recent in vivo analysis of more than 30,000 CAD/CAM ceramic restorations projected that in order to reach a 10% failure rate, IPS e.max inlays and onlays would need 124 years and 30 years, respectively.20 If such projections hold true, this would be a clear fulfillment of Mörmann's vision for the predictable restoration of teeth with durable esthetic restorations in a single visit with CAD/CAM technology.
Restorative material options for chairside CAD/CAM continue to expand. Following the current trend in laboratory-fabricated indirect restorations, several monolithic zirconia systems have been developed for chairside use, including IPS e.max ZirCAD® (Ivoclar Vivadent), CEREC Zirconia by Dentsply Sirona, Katana™ Zirconia by Kuraray Noritake Dental (kuraraynoritake.com), and BruxZir® Now by Glidewell Laboratories (glidewelldental.com). Of these materials, only BruxZir Now is milled in a fully sintered state, ready for polishing and delivery immediately after milling. The other zirconia options require sintering after milling, typically in a special oven that sinters the specially formulated zirconia much faster than traditional laboratory-sourced zirconia. Resin-ceramic hybrid materials have recently emerged on the market as well, such as Lava™ Ultimate from 3M (3m.com), Vita's Enamic®, Cerasmart® from GC (GCAmerica.com), and HC Block/Disk from Shofu (shofu.com). These materials have been developed in an attempt to combine the strength and durability of ceramics with the easy-to-manage and forgiving nature of resin composite. A zirconia-reinforced lithium-silicate material, Celtra® Duo (Dentsply Sirona), has also been developed, intended to give clinicians flexibility in the restorative material's management after milling (polished or fired), depending on the needed strength for the given clinical situation.
Practitioners should keep in mind that many of the newer hybrid materials and full-contour zirconia materials available for use have little or no data regarding their potential for clinical success. The same review and meta-analysis confirming the success of ceramic restorations urged caution in expecting the same of resin restorations. Several of the newer hybrid materials have failed to live up to manufacturer and user expectations.21,22 With the explosion of full-contour zirconia materials on the market, it is already well-documented that altering the characteristics of zirconia, for example to change esthetic properties, can significantly alter its physical properties and affect clinical performance.23 It would therefore be unwise to judge the potential for clinical success of newer zirconia formulations based on previous experience with original formulations of monolithic zirconia.
Today's Possibilities With Chairside CAD/CAM Systems
Perhaps the least interesting thing chairside CAD/CAM systems are capable of today is what they were originally intended for, ie, the chairside fabrication of an indirect restoration. With the entire scope of the dental profession moving into a digital realm, chairside CAD/CAM systems provide clinicians access to a new way to practice comprehensive dentistry. Digital workflows are quickly replacing conventional workflows in most aspects of dentistry, including diagnosis and treatment planning, smile design, the surgical placement and restoration of implants, and orthodontics.
Digital technology is not only great for diagnosis and treatment planning, it also allows that plan to be easily integrated into the restorative workflow. This is a distinct advantage over conventional workflows, especially in esthetic cases when it is critical to meet patient expectations. An illustration of this is a patient presenting with a desire to address his chipped maxillary incisors to make them more esthetic (Figure 1). Using digital photography, a retracted photograph of the patient's teeth was imported into smile-design software, which provided a quick and simple means of establishing a symmetrical restorative design for the patient (Figure 2). Within the same software, the proposed restorations were then overlaid on a full-face smiling photograph (Figure 3), and the patient was able to compare before-and-after photographs (Figure 4). The patient approved of the proposal, which was then imported into CAD software to facilitate fabrication of the final restorations based on the smile-design proposal (Figure 5).
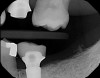
Plugging into digital workflows provides opportunities to integrate CAD/CAM technologies at every step of the treatment process for dental implants. In another example, a patient presented with a failing tooth No. 8 (Figure 6 and Figure 7). After discussing treatment options, the patient chose to forgo any treatment to address tooth and soft-tissue asymmetries and wanted to proceed with a dental implant-supported restoration without additional treatment. After integrated 3-dimensional planning, the tooth was extracted, and then an implant and the final custom CAD/CAM abutment (titanium base with zirconia supra-structure) were placed with a provisional restoration in the same visit (Figure 8 and Figure 9). Soft-tissue grafting was also done at the same visit to address the deficient buccal tissue height on No. 8 (Figure 10). At 3 months, the patient presented for the final restoration, with excellent healing around the implant (Figure 11) and soft-tissue healing guided by the custom abutment (Figure 12).
Integrative digital planning can also lead to quicker and more efficient treatment times for dental implant therapy. Another patient presented for a dental implant to replace tooth No. 19 at the end of orthodontic treatment. By leveraging 3D planning (Figure 13) and the printing of a surgical guide, the patient's implant was placed using a flapless approach. At the time of placement, an intraoral scan body was placed on the implant and digital impressions were made for her final restoration (Figure 14). At 10 weeks, the final custom abutment and CAD/CAM crown were delivered, all digitally fabricated without the use of physical models (Figure 15 through Figure 17). For implant placement and restoration, the patient had two visits, with a total chair time of 65 minutes, and no need for anesthetic at the second visit.
Digital impressioning and digitally driven treatment planning and execution are quickly becoming the norm in orthodontic treatment. This allows for interdisciplinary treatment to be performed digitally, even in the presence of brackets and wires. As an example, a 13-year-old patient presented with congenitally missing maxillary lateral incisors, as well as tooth No. 22. After discussing various treatment options, the patient and her parents decided to maintain the edentulous spaces with resin-bonded fixed partial dentures (RBFPDs) until the patient was old enough for dental implants. At completion of orthodontic treatment but before removal of brackets and wires, the patient was digitally scanned (Figure 18). Her models were manipulated in orthodontic software to remove the brackets, and the case was imported into restorative CAD software for design and fabrication of the RBFPDs (Figure 19). The e.max RBFPDs were milled and subsequently delivered immediately after bracket removal (Figure 20).
Conclusion
Digital dentistry and CAD/CAM are no longer experimental niche concepts. Chairside CAD/CAM has a proven track record of success, and the technology has evolved greatly since its initial inception. Today's chairside CAD/CAM is efficient, predictable, and easy to manage. In the same way these systems were originally designed to facilitate better restorative outcomes for patients in less time, they are now a significant contributor to facilitating better, faster outcomes for patients across the digital spectrum of dentistry. Patients can be treated interdisciplinarily in ways that shorten treatment times and reduce their number of visits, while matching or exceeding treatment outcomes achieved through conventional workflows. Whether treating one tooth or the whole patient, chairside CAD/CAM plugs today's clinician into the digital reality of 21st century dentistry.
About the Author
Clint Stevens, DDS
Private Practice
Tulsa, Oklahoma
References
1. Duret F, Preston JD. CAD/CAM imaging in dentistry. Curr Opin Dent. 1991;1(2):150-154.
2. Mörmann WH. The evolution of the CEREC system. J Am Dent Assoc. 2006;137 Suppl:7S-13S.
3. Fasbinder DJ. Clinical performance of chairside CAD/CAM restorations. J Am Dent Assoc. 2006; 137 Suppl:22S-31S.
4. Johnson R, Verrett R, Haney S, et al. Marginal gap of milled versus cast gold restorations. J Prosthodont. 2017;26(1):56-63.
5. Afify A, Haney S, Verrett R, et al. Marginal discrepancy of noble metal-ceramic fixed dental prosthesis frameworks fabricated by conventional and digital technologies. J Prosthet Dent. 2018;119(2):307.e1-307.e7.
6. Nawafleh NA, Mack F, Evans J, et al. Accuracy and reliability of methods to measure marginal adaptation of crowns and FDPs: a literature review. J Prosthodont. 2013;22(5):419-428.
7. Felton DA, Kanoy BE, Bayne SC, Wirthman GP. Effect of in vivo crown margin discrepancies on periodontal health. J Prosthet Dent. 1991;65(3):357-364.
8. Mounajjed R, Layton DM, Azar B. The marginal fit of E.max Press and E.max CAD lithium disilicate restorations: a critical review. Dent Mater J. 2016;35(6):835-844.
9. Manhart J, Chen H, Hamm G, Hickel R. Review of the clinical survival of direct and indirect restorations in posterior teeth of the permanent dentition. Oper Dent. 2004;29(5):481-508.
10. Renne W, Wolf B, Kessler R, et al. Evaluation of the marginal fit of CAD/CAM crowns fabricated using two different chairside CAD/CAM systems on preparations of varying quality. J Esthet Restor Dent. 2015;27(4):194-202.
11. Renne W, McGill ST, Forshee KV, et al. Predicting marginal fit of CAD/CAM crowns based on the presence or absence of common preparation errors. J Prosthet Dent. 2012;108(5):310-315.
12. Guess PC, Vagkopoulou T, Zhang Y, et al. Marginal and internal fit of heat pressed versus CAD/CAM fabricated all-ceramic onlays after exposure to thermo-mechanical fatigue. J Dent. 2014;42(4):199-209.
13. Borges GA, Faria JS, Agarwal P, et al. In vitro marginal fit of three all-ceramic crown systems before and after cementation. Oper Dent. 2012;37(6):641-649.
14. Renne W, Ludlow M, Fryml J, et al. Evaluation of the accuracy of 7 digital scanners: an in vitro analysis based on 3-dimensional comparisons. J Prosthet Dent. 2017;118(1):36-42.
15. Mennito AS, Evans ZP, Ludlow ME, Renne WG. Evaluation of the effect scan pattern has on the trueness and precision of six intraoral digital impression systems. J Esthet Restor Dent. 2018. doi: 10.1111/jerd.12371.
16. Tsirogiannis P, Reissmann DR, Heydecke G. Evaluation of the marginal fit of single-unit, complete-coverage ceramic restorations after digital and conventional impressions: a systematic review and meta-analysis. J Prosthet Dent. 2016;116(3):328-335.
17. Chochlidakis KM, Papaspyridakos P, Geminiani A, et al. Digital versus conventional impressions for fixed prosthodontics: a systematic review and meta-analysis. J Prosthet Dent. 2016;116(2):184-190.
18. Ahlholm P, Sipilä K, Vallittu P, et al. Digital versus conventional impressions in fixed prosthodontics: a review. J Prosthodont. 2018;27(1):35-41.
19. Morimoto S, Rebello de Sampaio FB, Braga MM, et al. Survival rate of resin and ceramic inlays, onlays, and overlays: a systematic review and meta-analysis. J Dent Res. 2016;95(9):985-994.
20. Belli R, Petschelt A, Hofner B, et al. Fracture rates and lifetime estimations of CAD/CAM all-ceramic restorations. J Dent Res. 2016;95(1):67-73.
21. Class 2 device recall Lava Ultimate. US Food & Drug Administration. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfres/res.cfm?id=137871. Published July 8, 2015. Updated April 5, 2018. Accessed April 6, 2018.
22. Fasbinder DJ, Vollmann M. Ensuring optimal clinical outcomes with Celtra Duo (ZLS) blocks for CEREC. CERECdoctors.com Magazine. 2018;Q1:26-30.
23. Christensen GJ. Translucent zirconias: tooth reduction and chairside adjustment issues. Clinician's Report. 2016;9(7):1-3.